What is Myopia?
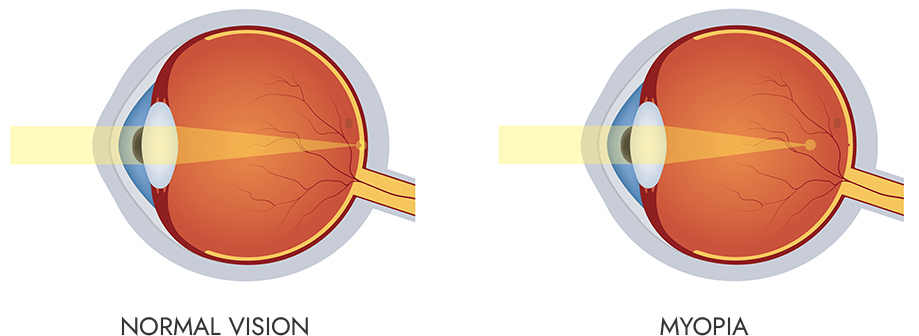
Myopia, also known as nearsightedness, is a common vision condition where you can see objects that are close clearly, but objects that are far away appear blurry.
Myopia is a rapidly increasing global health epidemic and one of the leading causes of vision impairment today.

What causes it?
Myopia usually occurs when:
The eyeball is too long relative to the focusing power of the cornea and lens.
Or the cornea is too curved for the length of the eye.
This causes light rays to focus in front of the retina (instead of directly on it), resulting in blurred distance vision.
Symptoms:
Blurry vision when looking at distant objects
Squinting to see clearly
Eye strain or headaches
Difficulty seeing the board at school
What is Myopia Management ?
Although myopia has historically been labeled as untreatable, innovations in ophthalmic optics, new research and studies now offer a chance to slow its progression in children with the condition.
Myopia management is especially important in children because myopia typically begins in childhood and often worsens as they grow. Without intervention, it can lead to high myopia, which significantly increases the risk of serious eye diseases later in life.
Here's why it's important:
Myopia tends to worsen with age
Children's eyes are still developing, so unchecked myopia can rapidly progress.
The earlier it starts, the more severe it can become.
High myopia increases risk of serious eye diseases. High myopia (usually worse than -6.00 diopters) is associated with:
Retinal Detachment/Retinal Tear
Glaucoma
Cataracts
Myopic Macular Degeneration
Impacts quality of life
Affects school performance, sports, extracurricular activities and social interactions, etc.
Leads to dependency on glasses or contact lenses at a young age.
Prevention is more effective than correction
While single vision glasses and soft contact lenses correct blurry vision, they don’t stop progression.
- Evidence-based myopia management methods (like orthokeratology, soft contact lenses, or special spectacle lenses) can slow down the progression by 30–60% or more.
Earlier intervention = better outcomes
Managing myopia early can lower the chance of your prescription progressing to high myopia, and help protect against long-term health risks.
- With new advances in medicine and technology, we can now detect ‘pre-myopia’ in children and begin intervention sooner.
FAQs
How are we able to properly track your child's myopic growth annually at SeaView Eyecare?
Our doctors have been successfully treating and monitoring myopic progression in children for years. Our myopia management protocols & programs are tailored and personalized to fit the specific needs of each child and their parents capabilities.
With proper care and state of the art technology, we are able to take precise measurements, track growth and generate reports with predicted growth charts that our parents can have access to.
What steps can I take from home?
Adopt the 2 hour rule- maximum of 2 hours a day of outside time a day (14 hrs each week) and maximum of 2 hours a day on screens. Also, correct minimum working distance while performing near tasks such as reading, homework, etc. This distance should be from the distance of your child’s chin to the end of their elbow when placing the palm of their hand under the chin.
How often should my child have an eye exam?
Your child should have a routine vision exam annually unless advised otherwise by the doctor per their individual treatment plan. If your child is enrolled in myopia management, the schedule will vary based on the type of management they are in. At minimum, the doctors will typically recommend a visit every 6 months in order to monitor for progression if at myopic risk. Treatment plans are individually based on level of care and/or intervention needed.
What ‘state of the art’ technology does SeaView Eyecare have?
At SeaView Eyecare, there are many different instruments we use in order to monitor for myopic progression. Some of the instruments we use include the OCULUS K5 Topographer for corneal mapping, iCare EIDON for retinal imaging, and the OCULUS Myopia Master to measure axial length (length of the eyeball) and monitor for change.
What additional options are available for myopia management?
Coming Soon...